Types of Fracture
Definition
A break in the continuity of bone which occurs when the bone is subjected to stress greater than it can absorb.
Causes
Diret blows
Crush injuries
Sudden twisting
Extreme muscle contractions
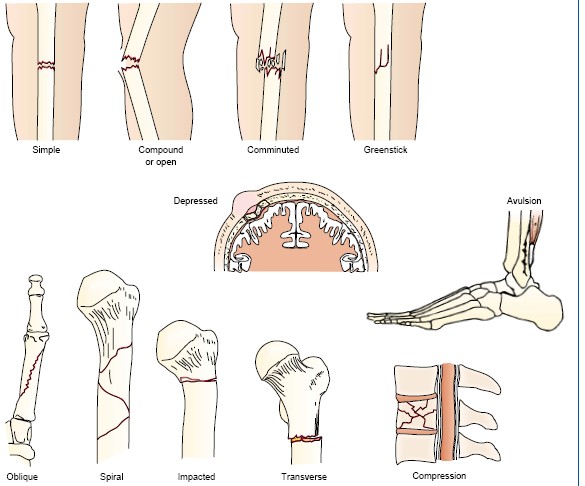
Types of fracture
Complete fracture : a break across the entire cross section of the bone often acccompanied by a displacement of the broken fragments
Incomplete fracture : only a part of the cross section involved
Cmminuted fracture : bone breaking into more than two fragments,
Closed fracture (Simple fracture) : no break in the skin
Open fracture (Compound) : break in the skin/mucous membrane occurs extending upto the bone
Complicated fracture : fracture damaging adjacent structures like nerves, muscles, blood vessels
Displaced fractures : the bone fragments out of normal alignment
Tranverse fracture
Oblique fracture
Green stick fracture : in young bone without breaking the continuity of the periosteal covering
Compression fracture (vertebral body)
Depression fracture (skull)
Impacted fracture
Avulsion fracture
Pathological fracture
Modalities of treatment of fracture
Closed reduction and immobilization
Open reduction and internal fixation
Immobilization with External Fixator
Bandaging
Immobilization with bandages, splints and POP
Skin traction or skeletal traction
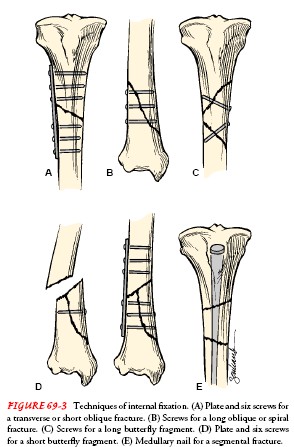
Techniques of Internal fixation
IM Nailing
Plate and screws
Lag screw
Dynamic srew
Dynamic hip screw
Hemiarthroplasty
Total replacement of jonts
Fixation with inlaying of bone grafts
Wiring
Factors that Enhance Fracture Healing
- Immobilization
- Maximum bone fragment contact
- Sufficient blood supply
- Proper nutrition
- Exercise for long bones
- Hormones : growth hormone, thyroid, calcitonin, vitamin D, anabolic steroids
- Electric potential across fracture
Factors that Inhibit Fracture Healing
- Extensive local trauma
- Bone loss
- Inadequate immobilization
- Space or tissue between bone fragments
- Infection
- Local malignancy
- Metabolic bone disease (eg. Paget's disease)
- irradiated bone (radiation necrosis)
- Avascular necrosis
- Intra-articular fracture (synovial fluid contains fibrolysins, which lyse the initial clot and retard clot formation)
- Age
- Corticosteroids (inhibit the repair rate)
Complications of Fracture
Shock
Fat embolism
Compartment syndrome
Deep vein thrombosis
Thomboembolism - pulmonary embolism
Disseminated intravascular coagulopathy
Infection
Damage to the adjacent important structures like nerves and muscles
Delayed union
Non union
Avascular necrosis of bone
Reaction to internal fixation devices
Complex regional pain syndrome
Heterotrophic ossification (myositis ossificans)
Deformity
Bone Healing
Bone healing or fracture healing is a proliferative physiological process
A fractured or broken bone undergoes repair through the following stages:
Reactive phase
Fracture and inflammatory phase - Granulation tissure formation Hematoma formation: hemorrhage, resulting in a hematoma
Bone cells deprived of nutrients begin to die.
Reparative phase
Cartilage callus formation - Lamellar bone deposition
Bone generation: Within days of the fracture, capillaries grow into the hematoma
while phagocytic cells begin to clear away the dead cells.
fragments of the blood clot may remain
Fibroblasts and osteoblasts enter the area and begin to reform bone.
Fibroblasts produce collagen fibers that connect the broken bone ends
Osteoblasts start to form spongy bone.
The repair tissue the fibrocartilaginous callus has both hyaline and fibrocartilage .
Bone spicules appear
Bony callous formation
The fibrocartilaginous callus is converted into a bony callus of spongy bone.
In two months for the broken bone ends are firmly joined together
The cartilage becomes ossified; osteoblasts, osteoclasts, and bone matrix are present.
Remodelling phase
Remodelling to original bone contour
Bone remodeling:
The bony callus is then remodelled by osteoclasts and osteoblasts
Excess material on the exterior of the bone and within the medullary cavity removed. Compact bone is added
This remodeling can take many months.